South Australian Medical Heritage Society Inc
Website for the Virtual Museum
Home
Coming meetings
Past meetings
About the Society
Main Galleries
Medicine
Surgery
Anaesthesia
X-rays
Hospitals,other organisations
Individuals of note
Small Galleries
Ethnic medicine
- Aboriginal
- Chinese
- Mediterran
Parkside Mental Hospital, 1954 To 1963
PRESENTED TO THE SAMHS BY DR. LOTHAR C. HOFF IN FEBRUARY 2013.
A FRANK, AS WAS, ACCOUNT OF MENTAL HOSPITALS AND THEIR STAFF MID LAST CENTURY.
Dr. Lothar C. Hoff, ED, MBBS, DPM (RCP&S), FRCMA, FRANZCP, MRC PSYCH. was born in 1927 at Koonibba in South Australia, where his father was the Pastor and Superintendent of the Koonibba Lutheran Mission. His early education was at the Adelaide High School and he studied Medicine at the University of Adelaide where he graduated in 1953. He was a first year intern at the Royal Adelaide Hospital and decided to become a Psychiatrist after attending a lecture about Psychiatry to the interns by Dr. John Cawte.
He started his duties at the Enfield Receiving House and the Parkside Mental Hospital (later called Glenside) in 1954. He obtained his DPM in London in 1960. He was a Superintendent at Parkside (1963-1980).
In 1971 he spent 3 months in Vietnam as an Army Reservist. His many appointments included numerous hospital committees. He was a Senior Visiting Psychiatrist at the Repatriation General Hospital, Acting Director of Mental Health Services in South Australia (1980-1985), and a member of the Guardianship Board (2002-2011). He was a foundation member of a committee which established the Sheltered Workshops for the handicapped, and attends a yearly function at Government House when the Lothar Hoff Award is presented to a company which supplied significant contracts to "Hands On".
His interests are in medical history, Glenside in particular. In 2004 he published his father's notes: "The Hoff Vocabularies of Indigenous Languages from the far West Coast of South Australia", (SKNZ Adelaide), and in 2008 donated his father's "The Hoff Collection" of 75 Aboriginal artefacts to the SA Museum (please see appendix). He is an active member of the SAMHS.
I have been associated with Parkside Mental Hospital, later renamed Glenside Hospital, for a long time, from 1954 to 1980. However, I will be restricting my remarks to Parkside Mental Hospital from 1954, when I began duties as a Medical Officer, to 1963, when there was a significant changing of the guard. Dr Birch retired in 1961. During 1962, Dr Cramond arrived from Scotland. In 1963, a new Superintendent was appointed. Also, I wish to briefly point out that, between 1954 and 1963, I was away for two years undertaking post-graduate training in London.
For completeness, it needs to be noted that in the early days of the colony, from 1836 to 1846, all disturbed people were admitted to the Adelaide Gaol. From 1846 to 1852, patients were admitted to the Public Colonial Lunatic Asylum, a small facility – a wooden house, eight rooms and cottages - sixty metres west of what is now the Water Tower in Conyngham Street, Glenside. In 1852, the Adelaide Lunatic Asylum was opened on the grounds of the present Botanic Gardens. By 1860, because of overcrowding, a Royal Commission was conducted and this resulted in a new building being started in 1866, and the first patients being admitted in 1870.
By way of background, in 1954, the main psychiatric facilities in South Australia were Parkside Mental Hospital, Northfield Mental Hospital and Enfield Receiving House. In addition, there were a couple of private psychiatric hospitals such as Fullarton Private Hospital and Karlyn. It also needs to be remembered that, in 1954, there were a few other hospitals, the notable ones being the Royal Adelaide Hospital, the Adelaide Children's Hospital, Queen Victoria Maternity Hospital, and Repatriation General Hospital. The Queen Elizabeth Hospital was opened in 1959, and was followed later by Flinders, Modbury and Lyell McEwen Hospitals. Many country towns had small hospitals. The main private hospitals were Calvary and Memorial.
It is also pertinent to remember how basic communication was at that particular time. I can remember reading that, in 1949, Prime Minister Ben Chifley was only able to speak by telephone to Premier Tom Playford during office hours. This was because the Norton Hills Post Office would have been closed down at nights and weekends. For this reason, Ben had a dedicated line put in, presumably from Adelaide Telephone Exchange to the Playford residence, so that he could speak to his friend, Tom, at any time of the day or night - no mobile phones in those days.
Also, 1954 was just nine years after World War II. The Playford Government was then well entrenched, and the emphasis was on building the state's infrastructure – namely, electrical power, roads, water reticulation, housing - particularly for ex-servicemen, and also to attract industry. Hospitals were relatively neglected, even the Royal Adelaide Hospital.
In 1954, Doctor Birch was the Superintendent of Mental Institutions and he had Deputy Superintendents at Parkside Mental Hospital, Enfield Receiving House, and Northfield Mental Hospital. In today's terminology, Dr Birch would have been the Director and Chief Advisor to the Minister of Health. But, Dr Birch had his office at Parkside and this meant that the Deputy Superintendent of Parkside had little autonomy. In 1954, Dr John Cawte was Deputy Superintendent of Enfield, and Dr Bill Salter of Northfield. Dr Brian Shea, who later became well known as the Director General, Medical Services in South Australia, was a Deputy Superintendent at Parkside for a time between 1954 and 1963. It's interesting to note that, at first, he did not have a higher degree.
So, how was it that I came to work at Parkside Mental Hospital? In 1953, Dr John Cawte spoke at a lunchtime meeting to the Resident Medical Officers at the Royal Adelaide Hospital about newly created opportunities to work in the mental institutions. Nothing was said about training opportunities, but the pay was very generous for the times, and also some housing was available. So, while on duty at the RAH in 1953, I telephoned the switchboard to absent myself, rode my 250cc motorbike to Parkside, was interviewed by Dr Birch and, as the saying goes, "the rest is history". However, as a medical student, I can recall honoraries advising against taking up psychiatry because "you become like the patients".
In 1954, Parkside was a "closed institution", surrounded by a high wall so the public couldn't look in. No doubt, this added to the fantasies about what happened inside. In actual fact, the wall was built to keep the public out so that people did not pinch things from the vegetable garden.
The following is an extract from page thirty-two of the book compiled and written by Henry T. Kay, 1870-1970, "Commemorating the Centenary of Glenside Hospital":
BOUNDARY WALL
Up to 1885, the Hospital property was fenced with post and wire fences only.During the proceedings of the Royal Commission held in 1884, the following recommendation was made:
"14. FENCING PARKSIDE ASYLUM GROUNDS – the evidence we have taken on this subject shows that a great many persons trespass on these grounds, that large quantities of vegetables, fruit and flowers are stolen every year, and that the patients are annoyed by the trespassers. With a view to preventing a continuance of these evils, your Commissioners beg to recommend that a suitable fence be erected round the grounds, with as little delay as possible.
Signed,
John Colton,
Chairman of Commissioners.
Executive Council Chamber, Adelaide,
July 21st 1884."
This is an appropriate time to acknowledge the aforementioned author, Mr Henry T. Kay J.P., who spent the whole of his working life (fifty years) at the Hospital. He commenced as a Messenger on the 2nd March, 1920 and retired as Lay Superintendent on the eve of his sixty-fifth birthday on the 1st March, 1970.
Parkside was a somewhat self-contained village, with its own administration area, a powerhouse which produced steam for the laundry and kitchen, a store, and it also had a small mortuary which is now being preserved as it is seen to be of great historic interest. Even in 1954, there was a sizeable wood heap, as internal fireplaces heated the wards and common rooms. There was a small tailor's shop, which not only would repair clothing, but was also used for the production of restraint garments for the disturbed patients. A small shop/canteen, which was privately run, was utilised by the visitors, staff and patients.
It was in the early 1960's that popular books were being written about the dangers of "closed institutions". At this point, I wish to introduce some statistics. The patient population in 1954 would have been about 1,700. The maximum daily inpatient occupation occurred on 23rd May 1958, when it reached 1,769 residents that night. This had dropped to about 1,400 in 1963. The single most important reason for this was the introduction of Chlorpromazine. In about 1958, I was seconded for a short period to Northfield Mental Hospital, later called Hillcrest Hospital. In one ward, with the complete encouragement of the Sister-in-Charge, I put just about every patient on Chlorpromazine or Largactil, which was produced by the pharmaceutical firm, May and Baker. Incidentally, the dosage was quite small, 25 mg TDS, and completely unlike the heavy doses of anti-psychotic medication dispensed now. Now, the end of this particular story is that sometime later, the drug representative of May and Baker told me that I, alone, was prescribing more Largactil than the whole state of Queensland.
Just to complete the broad brush of Parkside of 1954, the medical staff was limited to six, and of that six, two or three were retired General Practitioners, some of whom only attended to the physical aspects. There was one social worker whose duties included taking the photos of all new patients. There was one pharmacist who had one assistant. Within a year or two, a psychologist, Mr Pat Loftus, was appointed. There was, in total, approximately two hundred male and female attendants whose only qualification was a three year course which consisted of twelve one hour lectures per year. There was separation of male and female patients and staff, with the matron looking after the female half, and a chief male nurse looking after the male side. The roster for the "nursing staff" was two twelve hour shifts on consecutive days, alternating with two days off. The staff were very resistant to any changes to the roster.
Some of the female staff were registered nurses who took great pride in being able to assist in the small operating theatre. In fact, I can remember administering an ether anaesthetic, while a female patient was being operated on by Dr Leonard Lindon, who was performing a leucotomy. I can assure you that the procedure was not radical, and that the patient was greatly improved. I believe leucotomies were performed in private by surgeons such as Dr Dinning, Dr Escort-Hughes, and Dr L. C. Lindon. The first leucotomy in Australia was performed at Parkside.
In the overall picture of the mental health services, all new patients were admitted to Enfield Receiving House. Many became well enough to be discharged within a few weeks or, at most, a couple of months. Those with more chronic conditions were then directed to either Parkside or Northfield. It only needed one medical certificate to be admitted to Enfield, and then another single medical certificate to be admitted to a mental hospital. At that time, Dr Bill Salter of Northfield Mental Hospital had a special interest in the management of patients suffering from early schizophrenia, so it appeared that all the "good" patients were sent to Northfield, and those with more chronic conditions were sent to Parkside. There were a small number of voluntary patients, some who admitted themselves initially, and others who became voluntary patients when their illness remitted and, basically, they had nowhere else to go.
Patients contributed quite significantly to the unskilled labour needed in the running of the hospital. There were no domestics, and relatively few male and female attendants. So the patients did the house cleaning. Female patients worked in the laundry, and male patients in the kitchen, tailor's shop, the garden and the wood heap. In that sense, the hospital was quite economical to run.
I wish to acknowledge here, the work of Dr Hugh Birch. He came from an Adelaide family. As a youth, he experienced a motorbike accident resulting in partial paraplegia. Consequently, he always used a walking stick and walked with a shuffling gait. However, he was still able to drive his car and was fiercely independent. He had a higher degree - a Diploma of Psychological Medicine from London. His whole working life would have been spent at Parkside Mental Hospital as a Medical Officer, Deputy Superintendent and Superintendent. In 1962, I can recall him telling me that when he was a Medical Officer and had to do the night rounds of the hospital, he would have to administer tube feeds to six to twelve severely depressed patients, just to keep them alive. This, of course, magically ceased with the introduction of Electroconvulsive Therapy (ECT), which is still one of the most effective treatments for severe depression.
ECT was developed in 1938 by two Italian neuropsychiatrists, Ugo Cerletti and Lucino Binni, and gained widespread use as a form of treatment in the 1940's. But, owing to the outbreak of World War II in 1939, no machines were available in Australia, hence the need to construct a machine. Dr Birch wrote, "From meagre technical information given in various journals, a machine was built from bits and pieces of electrical equipment. Extreme caution was necessary as the apparatus was constructed by myself, a mere amateur, and not by any electro-medical company". He did submit this apparatus to Professor Kerr Grant of the Physics Department of the University of Adelaide. Another first – the first ECT performed in Australia was at Parkside Mental Hospital in 1940.
I wish now to relate a couple of anecdotes about Dr Birch's ability not to spend money unnecessarily:
Dr John Cawte wanted to hold an evening clinical meeting in one of the wards at Enfield Receiving House, so he telephoned Dr Birch seeking permission to install an overhead light to the entrance of the particular building. Dr Birch excused himself, and after a couple of minutes returned and stated, "Dr Cawte, I've consulted my almanac and there's a full moon that night." - end of conversation!
Now, I lived in a hospital house on the grounds, and when on-call at night or over the weekend, I was notified as required via the hospital switchboard. As I liked spending time in the garden, I requested that an outdoor bell be fitted as well. This was curtly refused saying that if I could not be alerted by phone, a hospital attendant would summons me. Also, I recall Dr Birch stating on one occasion: "The best committee is a committee of two, with one away".
Perhaps I can mention that when we lived in hospital houses off Greenhill Road, we never locked the house at night. The criminal element of society displayed the same prejudices and fears of the mental hospital, as the general public.
What about the patients? How did they adjust to their situation? Many were feeble and required care, equivalent to the levels needed in a current nursing home. But, of course, there was a huge contrast in the standard of the physical facilities. The facilities for the intellectually retarded were particularly poor. Sometimes, the elderly and intellectually retarded were not segregated, the theory being that the elderly would nurture the intellectually handicapped, with benefit to both parties. The standard of clothing was very poor indeed.
There was the odd obsessional patient who was highly valued by staff because they were extremely good workers. Often they were rewarded with extra tobacco ration or cigarettes. Only in later years was this withdrawn because of health reasons. Of course there was no social security.
At that time, all the case notes were kept centrally, in the main administration building. Visitors generally did not see inside the wards, but the patients were escorted to a central visiting room in the main building. Visiting hours were restricted to two hours, three days a week - from 2pm to 4pm on Wednesdays, Saturdays and Sundays.
As a generalisation, the staff were solicitous. As in any large organisation, there's always the possibility of misadventure. The union was powerful, and would automatically support any staff member charged with any offence, even to the point of paying legal expenses. Being a nurse or an attendant was a low-status job, and many were migrants from Europe, and some, of course, were quite educated people. They valued their jobs. Although not quite in this time period, selected for this presentation, the most famous male nurse must go to that of the late Mr John Gillard, the father of our former Prime Minister. I can remember him being a very good nurse, as well as being very literate, and once saying rather prophetically: "Politics is the ultimate theatre." He could quote from a book of famous speeches, delivered by eminent people such as Socrates, Lincoln, Churchill, and Martin Luther King.
What about the legal system? One good feature of the times was that many patients were granted day leave and also weekend leave to the oversight of a responsible person, usually a relative. When patients had improved, many were granted six months trial leave, at the end of which they would be automatically discharged. Similarly, if patients absconded, and had not been returned by the police within the six month period, they would be automatically discharged. Generally, the management of disturbed behaviour of psychiatric patients in the community was not popular with the police, who had the support of the government. For patients admitted under certificate, there was no automatic appeal system, although the Minister of Health did receive complaints.
In hindsight, I was very paternalistic. I think it is fair to say it was the general attitude of the community of the time. Once a patient's illness had remitted, they were discharged. However, if they subsequently relapsed, the public was not impressed and we did receive some flak.
In any institution there's always the considerable apprehension regarding suicide which, of course, was automatically reported to the police and coroner. Hence, efforts were made for those considered at risk, to receive closer supervision. I recall having to sign daily suicide cards, and in hindsight, we were excessively cautious. Also, at that stage, people who attempted suicide could, in theory, be charged with an offence, although I do not recall that ever happening. Between 1954 and 1963, there was increasing use of physical methods of treatment. In the distant past, Chloral Hydrate and Paraldehyde were used as sedatives. Reference has been made to Chlorpromazine or Largactil which, of course, was followed by Stelazine and Melleril and a whole host of psychotropic and anti-depressive medications. It is interesting to note that the drug companies were, at first, slow in developing anti-depressant and other anti-psychotic medications because it was thought not to be profitable.
ECT was, at first, administered without any anaesthetic, but later, the technique was developed where the solo doctor administering ECT would inject a fast acting barbiturate, and then, after the patient was well oxygenated, introduce an intravenous muscle relaxant such as Scoline. I can recall becoming quite adept at this procedure. Nowadays, no self-respecting psychiatrist would venture to administer ECT without a specialist anaesthetist.
I wish to conclude by commenting on the state of post-graduate education in those days, which was just about nil. Although there was an Association of Psychiatrists who held monthly meetings and Medical Officers were welcome, Bill Salter of Hillcrest, went to London for his training, while John Cawte of Enfield, went to Melbourne, and this required a three month residency. Raynor Smith and I went to England in 1960 and obtained a DPM (FRCS and FRCP). In the period 1954 to 1963, there was a very interesting perk for Medical Officers, no longer available. I understand that in the 1920's a Medical Officer working at a mental hospital committed suicide. As a consequence, a scheme was introduced so that after five years of service, a Medical Officer was granted six month's leave on full pay. With time accumulated from this scheme I was able to travel to England in the 1960's and South Vietnam in 1970. The perk was withdrawn in the 1960's.
Finally, I wish to draw to your attention the excellent photographic record of facilities for the management of the mentally ill from early colonial times to more recent times, prepared by Professor Robert Goldney and Mr David Buob, and which can be found on the SA Medical Heritage Society Inc. website on the page under the heading "Hospitals and other institutions", and listed below:
APPENDIX
Dr. Hoff has kindly provided several photographs from his publications which show his involvement in the history South Australia
A PAGE FROM DR. HOFF'S BOOK DEALING WITH HIS FATHER PASTOR BERNHART FRIEDRICH CARL'S NOTES ON NATIVE LANGUAGES.
PHOTOGRAPH OF DR. HOFF WITH DR. PHILLIP JONES FROM THE SOUTH AUSTRASLIAN MUSEUM NEWS LETTER APRIL/JUNE 2008 AT THE DONATION OF HIS FATHER'S 75 ABORIGINAL ARTEFACTS TO THE SA MUSEUM.
SOME OF THE ABORIGINAL ARTEFACTS ON PUBLIC DISPLAY DURING THE HOFF FAMILY'S VISIT TO THE NETLEY STORES. DR HOFF IS ON THE EXTREME LEFT.
PAGE 42 FROM PASTOR HOFF'S EXERCISE BOOK ABOUT NATIVE LANGUAGES FROM THE TRIBES IN THE FAR WEST COAST OF SOUTH AUSTRALIA. PUBLISHED BY DR. HOFF IN 2004.
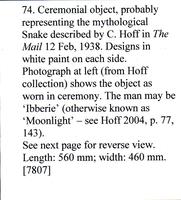
ORNAMENT USED AT CEREMONIES: IT WAS WORN IN FRONT OF THE FACE AND RESEMBLED A HALO.
PHOTO AND A COMMENT FROM DR. PHILLIP JONES ABOUT THE ABOVE ORNAMENT.
-o0o-